Hepatitis – an underestimated disease with a high number of unreported cases
First identified in the 1980s, AIDS and the underlying HIV infection developed into a pandemic that has killed an estimated 39 million people to date. Since 1996, when combination drugs were brought to market thanks to pharmaceutical research, the infection has been transformed from fatal to chronic disease, which has enabled them to lead a largely normal life.
Traced back to 100 years ago
The immunodeficiency virus likely first appeared 100 years ago when it jumped from a dead animal to a hunter via a cut and subsequently developed into the human immunodeficiency virus “HIV”. The virus is thought to have spread from Africa to the western world via Haiti in the 1960s. The rapid spread of the virus in the homosexual community ultimately led to the discovery of the disease in the 1970s, which is why it was initially referred to as “gay-related immune deficiency” (GRID). The HI virus mutates so quickly that more different virus variants develop in the body of an HIV-positive person every day than flu variants worldwide. Research into a vaccine, which has been ongoing since the 1980s, has therefore been unsuccessful so far. As a result, the disease is still considered incurable – however, thanks to advances in treatment, HIV is no longer a death sentence.
The development of HIV treatment: various breakthroughs in a very short time
HIV was first clinically observed in the United States in 1981. Since 1984 it is possible to use an antibody test to find out if a person carries the HI virus and it has been mandatory to test blood products for HIV antibodies since 1986. In 1985, the Japanese virologist Hiroaki Mitsuya demonstrated the effectiveness of the substance azidothymidine (AZT), originally developed as a cancer medication, and it was finally approved as the first HIV drug in the USA two years later. This milestone in the treatment of HIV infection made it possible for the first time to counteract the multiplication of HIV in the body and thereby increase the life expectancy of patients. In the late 1980s, it became possible to prescribe two other medications (didanosine and zalcitabine) before they were officially approved. In 1995, the first protease inhibitor was approved in the USA as a novel treatment approach. Eventually, in the mid-1990s, studies showed that combined treatment with two active substances worked better than monotreatment.1
The big breakthrough in HIV treatment came with antiretroviral combination treatment, whereby several drugs are combined. This form of treatment aims to permanently inhibit the multiplication of the HI virus. Combined treatments also remain effective in the long term, since the virus almost never succeeds in simultaneously developing resistance mutations against several medications.
Drug treatment of people with an HIV infection reduces viral load and maintains immune system function. If the viral load of an HIV-positive person can no longer be detected, the treatment is so successful that the patient is no longer infectious.2
While a positive HIV test still came as a certain death sentence before 1996, in most cases an HIV infection can now be transformed into a chronic disease3. This treatment breakthrough is also underpinned by impressive figures:
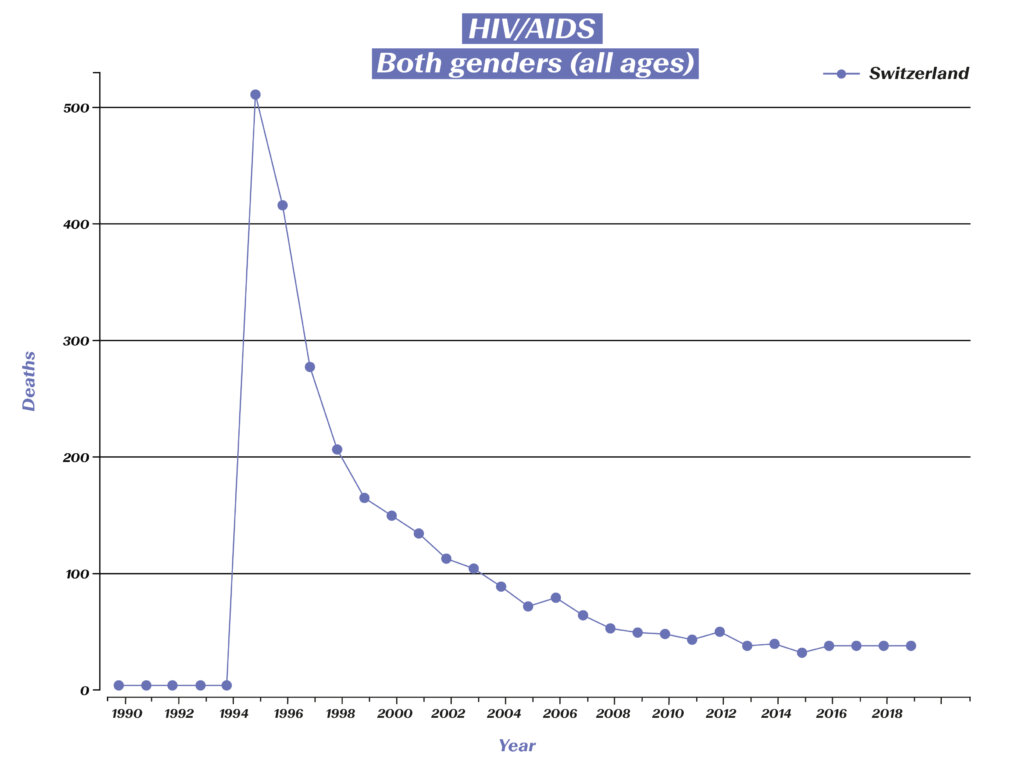
Deaths related to HIV/AIDS in Switzerland. (Source: Global Burden of Disease (GBD), https://vizhub.healthdata.org/gbd-compare/#)
While more than 500 HIV-related deaths were recorded in Switzerland in 1995, the number of deaths in recent years has been reduced to around 30. Those affected can live a long life, but this also means that they are dependent on medication for the rest of their lives, as it is impossible to eliminate the virus from the body after infection. Taking the medication as prescribed requires a high level of discipline on the part of the affected individual, therefore research has also made great strides in facilitating the regimen for patients. In the 1990s, a handful of drugs had to be taken at specific and precisely defined times. Now, just one pill a day is often sufficient. Compared to the previous treatment, modern medications also cause fewer side effects in many patients, which also contributes to improving the quality of life of those affected.
Infection prevention, active substances as prophylaxis and a glimpse into the future
Post-exposure prophylaxis (PEP) can now be used to prevent the virus from “implanting” after exposure, so that the exposed person remains HIV-negative. A PEP must be prescribed by a doctor, ideally within 24 hours and no later than 72 hours after exposure. The treatment must be continued for a period of four weeks; the treatment consists of regular HIV medication.
In 2016, a combination treatment in pill form for HIV prevention was approved in Europe. Since then, physicians have been permitted to prescribe the medication as pre-exposure prophylaxis (PrEP) to healthy adults with an increased risk of infection. Prescribing drugs as PrEP is considered part of an overall strategy to prevent HIV infection, which also includes regular doctor visits and check-ups combined with safer sex practices.
There are currently over 30 medications in eight different medicine classes available to combat HIV. Although we do not have a full cure for HIV infections yet, the example of HIV demonstrates how scientific research can be used to develop treatments and consistently improve them. Hope remains that rapid progress will continue in the coming years and that a cure will soon be found for HIV.
1 Magazin HIV (2011): 30 Jahre HIV – Chronik. https://magazin.hiv/magazin/gesellschaft-kultur/30-jahre-hiv-chronik-1981-1986/
2 Deutsche Aidshilfe (2022): HIV-Behandlung. https://www.aidshilfe.de/hiv-behandlung#:~:text=Bei%20einer%20HIV%2DBehandlung%20werden,die%20Bildung%20von%20Resistenzen%20verhindert
3 Universitätsspital Zürich (2022): Treatment of HIV-infection. https://www.usz.ch/en/clinic/infectiology/offer/treatment-of-hiv-infection/
HIV
HIV (abbreviation of human immunodeficiency virus) consists of two species of enveloped viruses from the retrovirus family. Untreated the infection leads to a progressive weakening of the immune system. The final stage of the disease is known as Acquired Immune Deficiency Syndrome (AIDS).
Infection with the virus usually occurs through unprotected sexual intercourse, but the virus can also be transmitted through contaminated needles in the context of intravenous drug use. Once the virus has entered the blood, it mainly infects certain white blood cells, which control the body’s immune responses.
According to current estimates, around 17,000 people in Switzerland are living with an HIV infection. The number of new infections has been falling steadily since 1997 but was still at 2 million infections worldwide in 2014.

