Heart attack – from fate to controllable disease
The symptoms of hepatitis were first described as early as the 5th century BCE. However, nobody knew where hepatitis came from or how to treat it at that time. Today effective vaccinations offer protection against hepatitis A and B. Although there is still no vaccination against hepatitis C, the chances of recovery are over 95% thanks to modern treatments.1
Unidentified for centuries
Reports of outbreaks of epidemic jaundice, a common consequence of hepatitis, date back to ancient times. However, it was not until the mid-20th century that it was discovered that hepatitis is mostly caused by viruses. In 1947, the British physician F.O. McCallum first made the distinction between hepatitis viruses A and B. In the late 1980s, researchers finally discovered the hepatitis C virus, which is often chronic and therefore considered the most dangerous hepatitis virus. An estimated 400 million people worldwide are infected with one of the virus variants, and over 1.3 million people die from the disease every year.2
Hepatitis can be treacherous because many symptoms occur gradually. It can often take years before those affected notice that they have been infected – with serious consequences for the liver.
Breakthrough vaccination against hepatitis
hepatitis A and B (also available as combination vaccine). The first hepatitis A vaccines were approved in Europe in 1991. They are now on the World Health Organization (WHO) List of Essential Medicines, as they offer protection against one of the most common infectious diseases in high-risk regions such as Africa, Asia, Central America and South America with an effectiveness rate of 95–99%. Vaccination is therefore recommended for all travelers visiting a country with a high prevalence of hepatitis A.3
Vaccination against the hepatitis B virus has been available since 1984. It is one of the primary vaccines in Switzerland and offers vaccinated people 10 years of immunity – with a booster in adulthood, this immunity even lasts for decades.4 The vaccination recommendation for adolescents, which the Federal Office of Public Health (FOPH) introduced in Switzerland in 1998,5 has significantly contributed to the steady decline in the number of new hepatitis B infections in Switzerland:
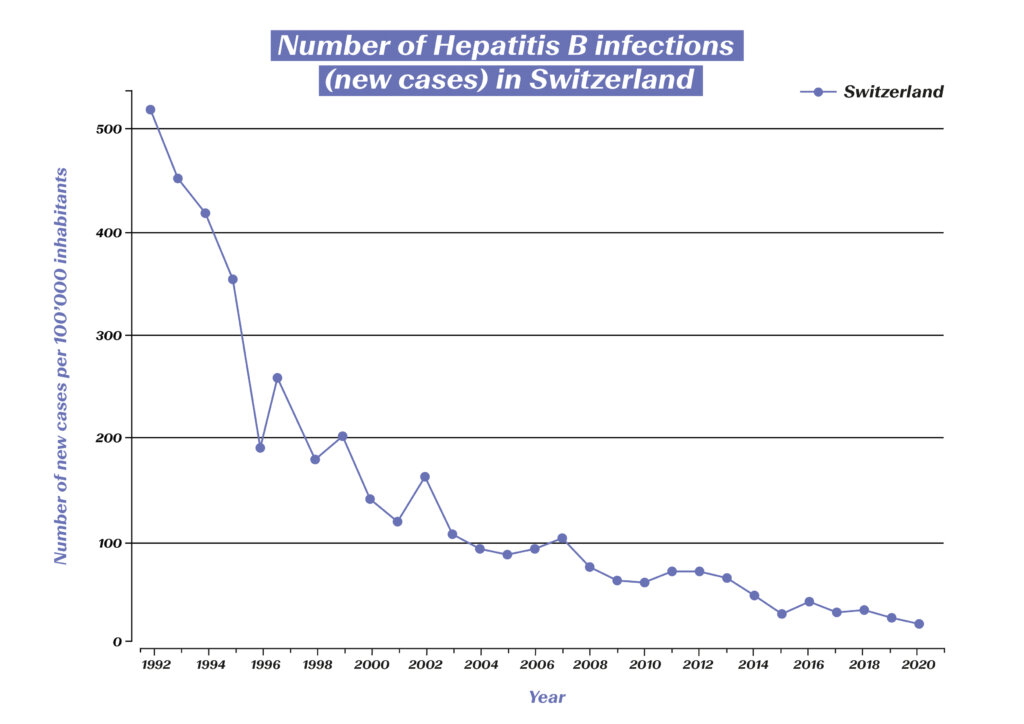
Number of hepatitis B infections (new cases) in Switzerland. (Source: Statista) https://de.statista.com/statistik/daten/studie/544724/umfrage/neuerkrankungen-an-hepatitis-b-in-der-schweiz/
Thanks to the high rate of immunization, the estimated global prevalence in children under the age of five has been reduced from 4.7% to below 1% over the past 40 years. Studies also show a threefold lower incidence of liver cancer caused by this virus variant among vaccinated people. The hepatitis B vaccine could therefore even be described as a vaccination against cancer.4
Advances in treatment thanks to targeted research
If infection with a hepatitis virus occurs and becomes chronic, this can have serious consequences and may lead to liver cirrhosis or liver cancer. While hepatitis A never becomes chronic, this can happen with both hepatitis B and C. Thanks to new developments in medical research, however, chronic disease can now be treated effectively.
In the event of a hepatitis B infection, antiviral agents are used which reduce the viral load in the blood, thereby preventing serious complications. In addition, new virological diagnostic methods are making it increasingly easy to determine the best treatment option.
Treatment of hepatitis C has come a long way since the virus was discovered in 1989. At first, patients were treated with interferons for six to 12 months. The cure rate was initially less than 20%, and involved considerable side effects for the patients. In the second decade, the cure rate was gradually increased to 45%, in part through the combination with ribavirin. Decisive progress has finally been made in the last two decades – the identification of the protein structure enabled the development of highly potent antiviral drugs with an excellent safety profile. In 2015, a breakthrough in cure rates and side effects was finally achieved with interferon-free treatment.6 Until recently, chronic hepatitis C was the most common cause of liver transplantation in Switzerland, but now 98% of all infections can be cured. On average, affected individuals are now virus free after just 8–12 weeks of treatment. As of 2022, all medications for the treatment of hepatitis C can be prescribed by doctors without restrictions.7 The treatments that have emerged through the power of biomedical research are now presenting a prospect long thought impossible: the global eradication of hepatitis C and thus of millions of human lives saved.
The WHO has therefore set itself the goal of global hepatitis B and C containment by 2030. The plan is to achieve this through a combination of different measures, but vaccines are the key to success. It can be expected that the rapid progress made in the development of COVID-19 vaccines will also boost the development of a vaccine against hepatitis C.8 Also, intensive research continues into even more effective treatment options for hepatitis B. In addition, the development of diagnostics continues to play a key role in the global fight against hepatitis.
1 Deutsches Bundesministerium für Bildung und Forschung (2019): Hepatitis – Eine unterschätzte Krankheit. https://www.gesundheitsforschung-bmbf.de/de/hepatitis-eine-unterschatzte-krankheit-mit-hoher-dunkelziffer-9689.php
2 Hepatitis Schweiz (2022): Was ist Hepatitis? https://hepatitis-schweiz.ch/formen/was-ist-hepatitis
3 Robert Koch Institut (2019): Hepatitis A. https://www.rki.de/DE/Content/Infekt/EpidBull/Merkblaetter/Ratgeber_HepatitisA.html
4 Gerlich, Wolfram H. (2022): Hepatitis-B-Impfstoffe – Geschichte, Erfolge, Herausforderungen und Perspektiven. Bundesgesundheitsblatt 65: 170–182.
5 Bundesamt für Gesundheit (2020): Impfungen – Zahlen und Fakten. https://www.bag.admin.ch/bag/de/home/strategie-und-politik/nationale-gesundheitsstrategien/nationale-strategie-impfungen-nsi/zahlen-fakten.html#:~:text=Schweizweit%20sind%2070%20Prozent%20der,von%2012%20bis%2089%20Prozent
6 Grätzel, Philipp (2019): Die Interferontherapie ist Geschichte. 13th Expert Summit on Viral Hepatitis, 10./11. Februar 2017, Berlin (Veranstalter: MSD). https://link.springer.com/content/pdf/10.1007/s15006-017-9415-x.pdf?pdf=button
7 Hepatitis Schweiz (2022): Neu können Hepatitis-C-Medikamente auch von Hausärzt:innen verschrieben werden. https://hepatitis-schweiz.ch/news/neu-koennen-hepatitis-c-medikamente-auch-von-hausaerztinnen-verschrieben-werden
8 Swiss Medical Forum (2022): Hepatitis C ist heilbar: eine Erfolgsgeschichte der biomedizinischen Forschung. https://medicalforum.ch/de/detail/doi/smf.2022.09003
Hepatitis
Hepatitis is an inflammation of the liver. It is always triggered by damage to or destruction of liver cells. This is usually due to infections with certain viruses, or less frequently due to toxins, alcohol or autoimmune diseases. The disease occurs acutely or chronically; in the acute case, the affected individual usually recovers within six months.
Several viral forms of hepatitis are known, showing differences in severity and duration. The most significant forms that also occur in Switzerland are hepatitis A, B and C, as well as hepatitis D (always occurs in connection with type B) and E.
Hepatitis A never becomes chronic, and usually heals completely resulting in lifelong immunity. It is transmitted through contaminated drinking water, contaminated food or smear infections and is also known as “traveler’s hepatitis”.
Hepatitis B is the most common liver disease in the world and is generally transmitted through unprotected sexual intercourse or blood and usually results in acute disease.
Hepatitis C, on the other hand, is becomes chronic in about 80% of cases. The most common forms of transmission are hypodermic needles during drug use or poor hygiene during medical procedures.

